The lipid profile is a blood test that measures the levels of different types of fats (lipids) in your blood. These lipids are essential for various bodily functions, including building healthy cells, producing hormones, and absorbing vitamins. However, when certain lipids are present in excessive amounts, they can become detrimental to your cardiovascular health.
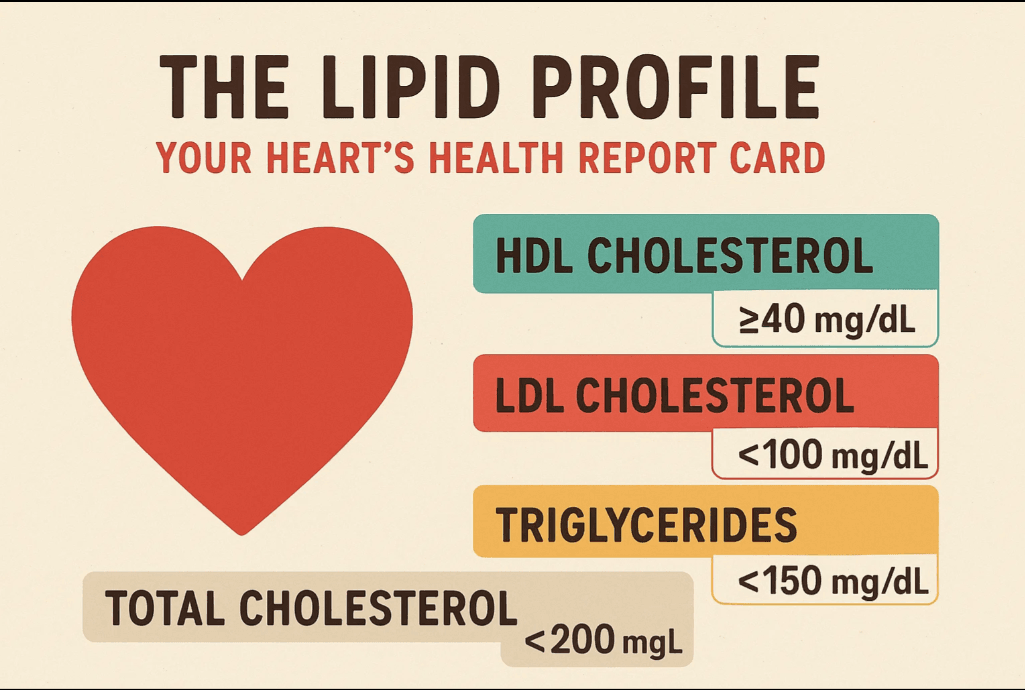
A standard lipid profile typically includes the following measurements:
- Total Cholesterol: This is the sum of all cholesterol in your blood.
- Low-Density Lipoprotein (LDL) Cholesterol: Often referred to as “bad” cholesterol.
- High-Density Lipoprotein (HDL) Cholesterol: Known as “good” cholesterol.
- Triglycerides: Another type of fat in your blood.
Understanding each component is vital for interpreting your lipid profile and taking appropriate action.
What is Cholesterol? Beyond the Buzzwords
Cholesterol is a waxy, fat-like substance that’s found in all the cells in your body. Your body needs cholesterol to make hormones, Vitamin D, and substances that help you digest food. Your body makes all the cholesterol it needs. However, you also get cholesterol from the foods you eat, particularly from animal products.
Cholesterol doesn’t travel freely through the bloodstream. Instead, it’s transported by particles called lipoproteins. These lipoproteins are the key to understanding “good” and “bad” cholesterol.
The “Bad” Cholesterol: Low-Density Lipoprotein (LDL)
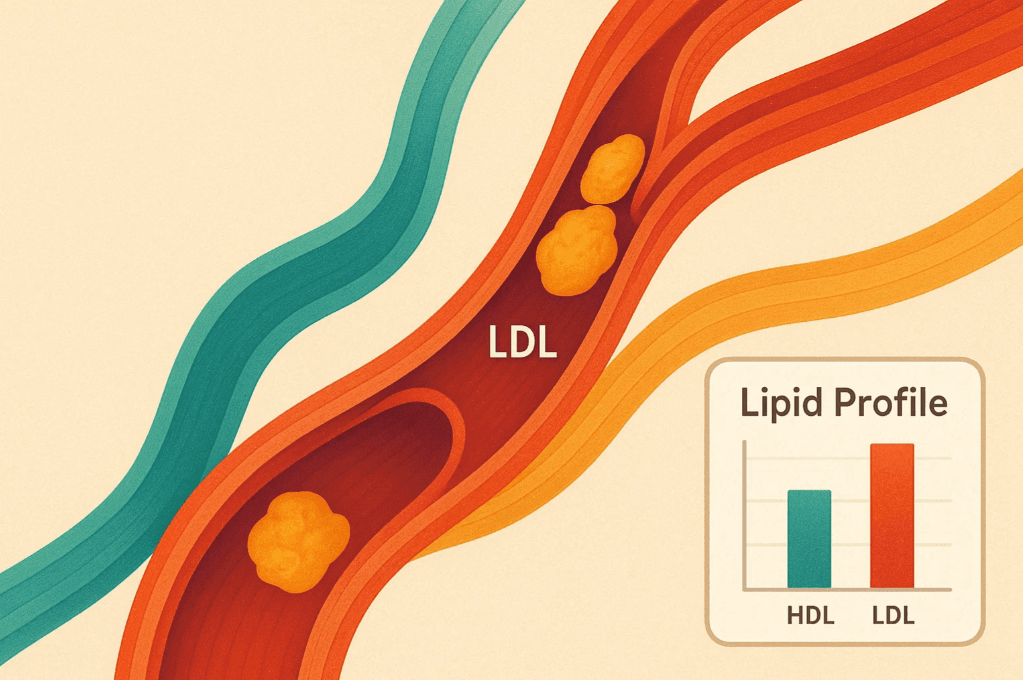
Low-Density Lipoprotein (LDL) cholesterol is often called “bad” cholesterol because high levels can lead to a buildup of plaque in your arteries. Think of LDL as the delivery truck that transports cholesterol from the liver to the body’s cells. When there’s too much LDL cholesterol, these “delivery trucks” can deposit cholesterol in the walls of your arteries.
This buildup, known as plaque, can narrow your arteries and make them less flexible (a condition called atherosclerosis). Over time, this hardening and narrowing of arteries can restrict blood flow to your heart and other organs, increasing your risk of:
- Coronary Artery Disease (CAD): Narrowing of the arteries that supply blood to the heart.
- Heart Attack: Occurs when blood flow to a part of the heart is blocked, usually by a blood clot formed on ruptured plaque.
- Stroke: Occurs when blood flow to a part of the brain is blocked, either by a clot or a ruptured blood vessel.
- Peripheral Artery Disease (PAD): Narrowing of arteries in the limbs, often the legs.
High LDL is a primary target for cholesterol-lowering strategies. Lipid Profile
The “Good” Cholesterol: High-Density Lipoprotein (HDL)
High-Density Lipoprotein (HDL) cholesterol is often referred to as “good” cholesterol. Think of HDL as the cleanup crew. It picks up excess cholesterol from various parts of the body and carries it back to the liver, where it’s processed and removed from the body.
Higher levels of HDL cholesterol are generally associated with a lower risk of heart disease because they help prevent the buildup of harmful plaque in the arteries. HDL acts as a protective factor, sweeping away the cholesterol that could otherwise contribute to atherosclerosis. Lipid Profile
The Third Player: Triglycerides
Triglycerides are the most common type of fat in your body. They store excess energy from your diet. When you eat, your body converts any calories it doesn’t need to use right away into triglycerides. These triglycerides are stored in your fat cells. Hormones release triglycerides for energy between meals. Lipid Profile
While essential for energy, high levels of triglycerides can be a significant concern, especially when combined with high LDL cholesterol or low HDL cholesterol. Elevated triglycerides are linked to an increased risk of heart disease, and very high levels (over 500 mg/dL) can increase the risk of pancreatitis (inflammation of the pancreas). Lipid Profile
Normal Ranges for Lipid Profile in India
It’s important to note that optimal lipid levels can vary slightly based on individual risk factors and your doctor’s assessment. However, general guidelines for a healthy lipid profile in India are:
- Total Cholesterol:
- Desirable: Less than 200 mg/dL
- Borderline High: 200-239 mg/dL
- High: 240 mg/dL or higher
- LDL Cholesterol:
- Optimal: Less than 100 mg/dL
- Near Optimal/Above Optimal: 100-129 mg/dL
- Borderline High: 130-159 mg/dL
- High: 160-189 mg/dL
- Very High: 190 mg/dL or higher
- For individuals with existing heart disease or very high risk, the target LDL might be even lower, often below 70 mg/dL.
- HDL Cholesterol:
- Low (Poor): Less than 40 mg/dL (for men) / Less than 50 mg/dL (for women)
- Better: 40-59 mg/dL
- Optimal (Protective): 60 mg/dL or higher
- Triglycerides:
- Normal: Less than 150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: 500 mg/dL or higher
Note: A fasting lipid profile (typically 9-12 hours of fasting) is usually recommended for accurate results. Always consult your healthcare provider for personalized interpretation of your lipid profile. Lipid Profile
Why High Cholesterol is a Silent Threat: Risks and Complications
High cholesterol, particularly elevated LDL and triglycerides, is often called a “silent killer” because it typically has no noticeable symptoms in its early stages. You can have high cholesterol for years without knowing it, all while damage to your arteries accumulates. The first symptom might be a serious event like a heart attack or stroke. Lipid Profile
Symptoms (When They Do Appear)
While high cholesterol itself is asymptomatic, its long-term effects can manifest in symptoms related to its complications:
- Chest Pain (Angina): If the arteries supplying blood to your heart (coronary arteries) become narrowed due to plaque buildup, you might experience chest pain, pressure, or tightness, especially during exertion.
- Symptoms of Heart Attack: If a plaque ruptures and a blood clot blocks an artery completely, it leads to a heart attack. Symptoms include severe chest pain (often spreading to the arm, back, neck, jaw, or stomach), shortness of breath, cold sweat, nausea, or lightheadedness.
- Symptoms of Stroke: A stroke occurs when blood flow to the brain is interrupted. Symptoms can include sudden weakness or numbness on one side of the body (face, arm, leg), sudden vision problems, sudden severe headache, dizziness, or trouble speaking or understanding speech.
- Xanthomas or Xanthelasma: In rare cases of very high cholesterol (often genetic), yellowish fatty deposits may appear on the skin, especially around the eyes (xanthelasma) or on tendons (xanthomas).
- Arcus Senilis: A white or gray arc around the outer edge of the cornea of the eye can sometimes indicate high cholesterol, though it’s more common with age regardless of cholesterol levels.
Risk Factors for Unhealthy Lipid Levels
Several factors can increase your risk of developing unhealthy lipid levels:
- Unhealthy Diet:
- Saturated Fats: Found primarily in red meat, processed meats, full-fat dairy products (butter, cheese, whole milk), and some tropical oils (coconut oil, palm oil). These raise LDL cholesterol.
- Trans Fats: Often found in fried foods, baked goods (cookies, cakes, pastries), and some margarines. Trans fats raise LDL cholesterol and can also lower HDL cholesterol.
- High Cholesterol Foods: While dietary cholesterol has less impact than saturated/trans fats for most people, excessive intake from sources like organ meats, egg yolks (in large quantities), and shellfish can contribute.
- Excessive Sugar and Refined Carbohydrates: A diet high in added sugars and refined carbs (white bread, white rice, sugary drinks) can significantly raise triglyceride levels and lower HDL.
- Lack of Physical Activity: Inactivity lowers HDL cholesterol and can contribute to weight gain, which negatively impacts lipid levels.
- Obesity/Overweight: Carrying excess weight, especially around the waist, contributes to higher LDL and triglyceride levels and lower HDL.
- Smoking: Cigarette smoking damages blood vessels, lowers HDL cholesterol, and makes LDL cholesterol more likely to stick to artery walls.
- Excessive Alcohol Consumption: While moderate alcohol intake has been linked to slightly higher HDL, excessive drinking can significantly raise triglyceride levels and negatively impact overall heart health.
- Age: As you age, your liver becomes less efficient at removing LDL cholesterol from the blood, leading to naturally higher levels.
- Sex: Before menopause, women tend to have lower LDL levels than men. After menopause, women’s LDL levels often rise.
- Genetics/Family History: If close family members (parents, siblings) have a history of high cholesterol or early heart disease, you have a higher genetic predisposition. Conditions like Familial Hypercholesterolemia (FH) can cause extremely high cholesterol levels from a young age.
- Underlying Medical Conditions: Certain conditions can influence lipid levels, including:
- Diabetes (poorly controlled diabetes often leads to high triglycerides and low HDL).
- Hypothyroidism (underactive thyroid).
- Kidney disease.
- Liver disease.
- Polycystic Ovary Syndrome (PCOS).
- Sleep apnea.
- Certain Medications: Some drugs, like corticosteroids, certain blood pressure medications, and HIV/AIDS treatments, can raise cholesterol levels.
Complications of Unmanaged High Cholesterol
The primary and most dangerous complication of high cholesterol is atherosclerosis. Over time, this leads to:
- Heart Attack and Stroke: As discussed above, these are life-threatening emergencies.
- Angina (Chest Pain): Reduced blood flow to the heart muscle causes pain.
- Peripheral Artery Disease (PAD): Narrowed arteries in the legs and arms, causing pain, numbness, or cramping.
- Kidney Disease: Atherosclerosis can also affect the arteries leading to the kidneys, potentially impairing kidney function.
- Aortic Aneurysm: Weakening and bulging of the aorta, the body’s main artery, which can be life-threatening if it ruptures.
Mastering Your Lipid Profile: Comprehensive Management Strategies
Managing your lipid profile effectively requires a multi-pronged approach that combines significant lifestyle modifications with, if necessary, medical interventions. The goal is to lower LDL (“bad”) cholesterol and triglycerides while increasing HDL (“good”) cholesterol to protect your heart. Lipid Profile
I. Dietary Interventions: Eating Your Way to a Healthy Heart
Diet plays a pivotal role in cholesterol management. Small, consistent changes can yield significant results. Lipid Profile
- Reduce Saturated and Trans Fats: This is arguably the most impactful dietary change.
- Saturated Fats:
- Limit: Red meat (especially fatty cuts like lamb, pork, and highly marbled beef), processed meats (sausages, bacon, deli meats), full-fat dairy products (butter, ghee, whole milk, cream, cheese), and tropical oils (coconut oil, palm oil).
- Choose: Lean cuts of poultry (without skin), fish, plant-based proteins (beans, lentils, tofu), and low-fat dairy options.
- Trans Fats:
- Eliminate: These are often found in partially hydrogenated vegetable oils. Check food labels for “partially hydrogenated oil.” They are common in many commercially baked goods (cookies, cakes, pastries), fried fast food, and some packaged snacks.
- Many countries, including India, are implementing bans or strict regulations on trans fats, but it’s still crucial to be vigilant.
- Saturated Fats:
- Increase Soluble Fiber: Soluble fiber can reduce the absorption of cholesterol into your bloodstream.
- Excellent Sources: Oats (oatmeal, oat bran), barley, beans (kidney beans, black beans, chickpeas), lentils, fruits (apples, pears, berries, citrus fruits), and vegetables (Brussels sprouts, carrots, broccoli).
- How it Works: Soluble fiber forms a gel-like substance in your digestive tract, which binds to cholesterol and prevents its absorption, carrying it out of the body.
- Incorporate Omega-3 Fatty Acids: While omega-3s primarily help lower triglycerides and have other heart-healthy benefits (like reducing blood pressure and inflammation), they are an important part of a heart-healthy diet.
- Fatty Fish: Salmon, mackerel, sardines, herring, and trout are excellent sources. Aim for at least two servings per week.
- Plant-Based Sources: Flaxseeds (ground flaxseeds are more effective), chia seeds, walnuts, and canola oil.
- Fish oil supplements can be considered, but always consult your doctor before starting any supplement.
- Embrace Healthy Unsaturated Fats: Replace unhealthy fats with monounsaturated and polyunsaturated fats.
- Monounsaturated Fats: Olive oil, canola oil, avocado, nuts (almonds, cashews, pecans), and seeds.
- Polyunsaturated Fats: Sunflower oil, corn oil, soybean oil, flaxseed oil, walnuts, and sunflower seeds.
- Caution: Even healthy fats are high in calories, so consume them in moderation.
- Limit Dietary Cholesterol: While less impactful than saturated/trans fats for most, if you have high cholesterol or certain genetic predispositions, limiting dietary cholesterol (found in animal products like egg yolks, organ meats, and shellfish) may still be beneficial. Aim for less than 200 mg per day if advised by your doctor.
- Reduce Added Sugars and Refined Carbohydrates: A diet high in these can significantly increase triglyceride levels.
- Limit: Sugary drinks (soda, sweetened juices), candies, pastries, white bread, white rice (opt for brown rice or millets), and highly processed foods.
- Choose: Whole grains (brown rice, whole wheat, quinoa, millets like jowar, bajra, ragi), fresh fruits, and vegetables.
- Consider Plant Sterols or Stanols: These substances, naturally found in small amounts in plants, can help block the absorption of cholesterol from the intestine. They are sometimes added to fortified foods like certain margarines, yogurts, and orange juice.
II. Lifestyle Modifications: Holistic Approach to Heart Health
Beyond diet, several lifestyle changes are crucial for managing your lipid profile.
- Regular Physical Activity: Exercise is a powerful tool for improving cholesterol levels.
- Benefits: It helps increase HDL (“good”) cholesterol, lowers triglycerides, and can also contribute to modest reductions in LDL. Regular exercise also aids in weight management and improves overall cardiovascular fitness.
- Recommendation: Aim for at least 150 minutes of moderate-intensity aerobic activity per week (e.g., brisk walking, jogging, cycling, swimming) or 75 minutes of vigorous-intensity activity. This can be broken into 30 minutes, five days a week. Incorporate strength training two or more days a week.
- Start Slow: If you’re new to exercise, begin with shorter durations and gradually increase intensity and time. Even short bursts of activity throughout the day (taking stairs, walking during lunch breaks) can add up.
- Achieve and Maintain a Healthy Weight: Losing even a few extra pounds can significantly improve your lipid profile.
- Benefits: Weight loss helps lower LDL cholesterol and triglycerides and can boost HDL. Excess fat, especially around the waist (visceral fat), is metabolically active and can negatively impact lipid levels.
- Strategies: Combine a calorie-controlled, heart-healthy diet with regular physical activity. Focus on sustainable changes rather than crash diets.
- Quit Smoking: This is one of the most impactful changes you can make for your heart health.
- Benefits: Quitting smoking rapidly improves HDL cholesterol levels. Within 20 minutes, your blood pressure and heart rate improve. Within a year, your risk of heart disease is halved.
- Support: Seek support from your doctor, family, and support groups to help you quit.
- Moderate Alcohol Consumption: If you drink alcohol, do so in moderation.
- Moderation: Up to one drink per day for women of all ages and men over 65, and up to two drinks per day for men 65 and younger.
- Caution: Excessive alcohol intake significantly raises triglyceride levels and can lead to other health problems. If you don’t drink, don’t start for potential cholesterol benefits.
- Manage Stress: Chronic stress can contribute to higher cholesterol levels.
- Mechanism: Stress hormones like cortisol can influence lipid metabolism.
- Techniques: Incorporate stress-reducing activities into your daily routine:
- Yoga and meditation
- Deep breathing exercises
- Spending time in nature
- Hobbies and social interactions
- Adequate sleep
- Prioritize Quality Sleep: Poor sleep patterns have been linked to unhealthy cholesterol levels.
- Recommendation: Aim for 7-9 hours of quality sleep per night.
- Strategies: Establish a regular sleep schedule, create a comfortable sleep environment, and avoid screens before bedtime.
III. Medical Interventions: When Lifestyle Isn’t Enough
Despite diligent lifestyle efforts, some individuals may still have high cholesterol due to genetic predisposition or other factors. In such cases, medication may be necessary. Always consult your doctor to determine the appropriate course of treatment.
Common types of cholesterol-lowering medications in India include:
- Statins: These are the most commonly prescribed and effective cholesterol-lowering drugs.
- Mechanism: Statins work by blocking an enzyme in the liver that produces cholesterol, thereby reducing the amount of cholesterol the liver makes. This leads to a decrease in LDL cholesterol. They also have anti-inflammatory effects that can stabilize plaque.
- Examples: Atorvastatin, Rosuvastatin, Simvastatin, Pravastatin, Lovastatin.
- Side Effects: Generally well-tolerated, but can include muscle pain, digestive issues, and in rare cases, liver problems or increased blood sugar.
- Cholesterol Absorption Inhibitors (e.g., Ezetimibe):
- Mechanism: These medications work by reducing the absorption of dietary cholesterol from the small intestine. They are often used in combination with statins or for individuals who cannot tolerate statins.
- PCSK9 Inhibitors (e.g., Evolocumab, Alirocumab):
- Mechanism: A newer class of injectable drugs that dramatically lower LDL cholesterol by enabling the liver to remove more LDL cholesterol from the blood. They are typically used for individuals with very high LDL (often due to genetic conditions) or those who cannot tolerate or don’t respond well to statins.
- Fibrates:
- Mechanism: Primarily used to lower high triglyceride levels and can also modestly increase HDL cholesterol. They work by affecting how the liver processes lipids.
- Examples: Gemfibrozil, Fenofibrate.
- Niacin (Nicotinic Acid):
- Mechanism: A B vitamin that can significantly raise HDL cholesterol and lower triglycerides and LDL cholesterol.
- Caution: High doses can cause uncomfortable side effects like flushing, and its use is now less common due to newer, more effective drugs and potential side effects at doses required for lipid modification.
- Bile Acid Sequestrants (Resins):
- Mechanism: These drugs bind to bile acids in the intestine, preventing their reabsorption. The liver then has to use more cholesterol to make new bile acids, thereby lowering blood cholesterol levels.
Important Considerations for Medication:
- Adherence: Taking medications as prescribed is crucial for their effectiveness.
- Regular Monitoring: Your doctor will regularly monitor your lipid levels and liver function (for statins) to ensure the medication is working and to manage any side effects.
- Combination Therapy: Sometimes, a combination of medications is used to achieve target lipid levels.
- Lifestyle is Still Key: Even with medication, maintaining a heart-healthy lifestyle (diet, exercise, weight management) is vital for maximizing benefits and overall cardiovascular health.
A Deeper Dive into Dietary Choices: What to Eat and What to Limit
Let’s expand on specific food groups to guide your dietary choices for a healthier lipid profile.
Foods to Embrace (Cholesterol-Friendly Choices):
- Whole Grains:
- Why: Rich in soluble fiber.
- Examples: Oats, barley, brown rice, whole wheat bread/pasta, quinoa, millets (jowar, bajra, ragi).
- Tip: Start your day with a bowl of oatmeal or include whole grains in at least half of your meals.
- Fruits and Vegetables:
- Why: Packed with soluble fiber, antioxidants, vitamins, and minerals. Naturally low in saturated fat and cholesterol.
- Examples: Apples, pears, berries, citrus fruits, green leafy vegetables (spinach, kale), broccoli, carrots, Brussels sprouts, beans, lentils.
- Tip: Aim for at least 5-7 servings a day. Incorporate them into every meal and as snacks.
- Legumes (Beans and Lentils):
- Why: Excellent source of soluble fiber and plant-based protein.
- Examples: Kidney beans, black beans, chickpeas (chana), various dals (toor, moong, masoor).
- Tip: Add them to soups, stews, salads, or make them a staple in your curries.
- Nuts and Seeds:
- Why: Contain healthy monounsaturated and polyunsaturated fats, fiber, and plant sterols.
- Examples: Almonds, walnuts, chia seeds, flaxseeds, sunflower seeds, pumpkin seeds.
- Caution: High in calories, so consume in moderation (a small handful daily).
- Fatty Fish:
- Why: Rich in Omega-3 fatty acids.
- Examples: Salmon, mackerel, sardines, herring.
- Tip: Aim for 2-3 servings per week. Choose baked, grilled, or steamed preparations over fried.
- Healthy Oils:
- Why: Good sources of unsaturated fats.
- Examples: Olive oil (extra virgin for cold use), canola oil, rice bran oil (common in India), sunflower oil.
- Tip: Use them for cooking and in salad dressings in moderation.
- Plant Sterol/Stanol Fortified Foods:
- Why: Can actively help lower LDL cholesterol by blocking absorption.
- Examples: Some fortified margarines, yogurts, and orange juices. Check labels specifically for “plant sterols” or “stanols.”
- Whey Protein:
- Why: Studies suggest whey protein, found in dairy products, may lower both LDL cholesterol and total cholesterol.
- Tip: Can be consumed as a supplement or from dairy sources.
Foods to Limit or Avoid (Cholesterol Caution):
- Red and Processed Meats:
- Why: High in saturated fat and cholesterol. Processed meats also often contain high sodium and unhealthy additives.
- Examples: Fatty cuts of beef, lamb, pork, bacon, sausage, hot dogs, deli meats.
- Tip: Choose leaner cuts, opt for poultry (skinless), fish, or plant-based proteins more often.
- Full-Fat Dairy Products:
- Why: High in saturated fat.
- Examples: Whole milk, cream, butter, full-fat cheese, ghee (though moderation of pure ghee can be okay for some).
- Tip: Switch to low-fat or skim milk, low-fat yogurt, and use butter/ghee sparingly.
- Deep-Fried Foods:
- Why: Often cooked in unhealthy oils (which can become trans fats when reused) and absorb a lot of fat.
- Examples: Samosas, pakoras, French fries, fried chicken, fried snacks.
- Tip: Opt for baked, grilled, roasted, or steamed preparations.
- Baked Goods and Sweets:
- Why: Often contain saturated fats, trans fats (in some commercial products), and high amounts of added sugars, which elevate triglycerides.
- Examples: Commercial cookies, cakes, pastries, donuts, mithai (Indian sweets) made with excessive ghee/sugar.
- Tip: Enjoy these as occasional treats. Opt for homemade versions with healthier ingredients or fruits for sweetness.
- Highly Processed Foods:
- Why: Tend to be high in unhealthy fats, sodium, and added sugars, and low in fiber and nutrients.
- Examples: Packaged snacks, instant noodles, many frozen dinners, sugary cereals.
- Tip: Focus on whole, unprocessed foods.
- Certain Tropical Oils (Coconut and Palm Oil):
- Why: While often marketed as healthy, these are high in saturated fat and can raise LDL cholesterol.
- Tip: Use sparingly or in moderation. Opt for healthier cooking oils like olive, canola, or rice bran oil.
Monitoring and Prevention: A Lifelong Commitment
Managing your lipid profile isn’t a one-time fix; it’s a lifelong commitment to a heart-healthy lifestyle.
Regular Screening
Regular lipid profile screening is essential, especially if you have risk factors.
- Adults: Generally recommended every 4-6 years for healthy adults.
- Individuals with Risk Factors: More frequent screening may be advised (e.g., annually) for those with a family history of heart disease, obesity, diabetes, high blood pressure, or existing cardiovascular conditions.
- Children and Adolescents: Screening may be recommended if they have a family history of high cholesterol or early heart disease.
Indian Context and Guidelines
In India, cardiovascular diseases are a significant public health burden. Guidelines emphasize early screening, particularly given the rising prevalence of lifestyle-related diseases like diabetes and obesity. Indian dietary patterns, often rich in fried foods, refined carbohydrates, and saturated fats (like excessive ghee in some preparations), can contribute to unhealthy lipid profiles. Therefore, culturally appropriate dietary advice and lifestyle modifications are crucial.
The latest guidelines for cholesterol management often emphasize a personalized approach, considering age-specific recommendations and risk assessment tools. While medication is crucial in many cases, daily routines centered on lifestyle modifications are equally important for improving cholesterol profiles, enhancing medication efficacy, and promoting overall well-being.
The Role of Your Doctor
Your doctor is your most important partner in managing your lipid profile.
- Interpretation: They will interpret your test results in the context of your overall health, medical history, and other risk factors.
- Personalized Plan: They will help you develop a personalized management plan, which may include dietary recommendations, exercise prescriptions, and if necessary, medication.
- Monitoring: They will monitor your progress and adjust your treatment plan as needed.
- Addressing Co-morbidities: They will also address any underlying medical conditions (like diabetes or high blood pressure) that can impact your lipid levels.
Conclusion: Empowering Yourself for a Heart-Healthy Future
Understanding your lipid profile – the intricate balance of good cholesterol, bad cholesterol, and triglycerides – is fundamental to safeguarding your cardiovascular health. High levels of LDL cholesterol and triglycerides, coupled with low levels of HDL cholesterol, silently pave the way for serious conditions like heart attacks and strokes.
The good news is that you hold significant power in influencing your lipid profile. By embracing a heart-healthy lifestyle – prioritizing a balanced diet rich in soluble fiber, healthy fats, and whole grains, engaging in regular physical activity, maintaining a healthy weight, quitting smoking, managing stress, and ensuring adequate sleep – you can make profound improvements. For many, these lifestyle changes alone are sufficient to bring lipid levels into a healthy range. For others, particularly those with genetic predispositions or significant risk factors, medical intervention in conjunction with lifestyle adjustments offers the best pathway to optimal heart health.
Remember, managing your lipid profile is an ongoing journey, not a destination. Regular check-ups, open communication with your healthcare provider, and a steadfast commitment to healthy living are your strongest allies in this endeavor. By taking proactive steps today, you empower yourself to live a longer, healthier, and more vibrant life, protecting your most vital organ – your heart.
🌐 The Power of Our District PR Ecosystem
We are not just a media agency—we are building an entire district-level digital infrastructure with:
Each site provides:
- SEO blog space
- Video PR hosting
- Local business features
- Event coverage
- News updates
Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile Lipid Profile, Lipid Profile, Lipid Profile, Lipid Profile
- Why High Cholesterol is a Silent Threat: Risks and Complications
- Mastering Your Lipid Profile: Comprehensive Management Strategies
- A Deeper Dive into Dietary Choices: What to Eat and What to Limit
- Monitoring and Prevention: A Lifelong Commitment
- Conclusion: Empowering Yourself for a Heart-Healthy Future
- 🌐 The Power of Our District PR Ecosystem